A gastroenterologist shares 5 top foods that help you p0op, including one that 'jump-starts the gut' in minutes
Stuck in pur-gut-ory?
In 2012, a 38-year-old mother of two, Kelly Barta, had recently stopped using the topical steroids she had relied on for nearly three decades to treat her eczema. Within days of quitting, her skin turned bright red, accompanied by intense pain and an unrelenting, deep-rooted itch.
“It felt like someone poured boiling water over my entire body,” Barta recounted. The burning sensation persisted for five years, during which she lost her career, her marriage, and almost her life.
Barta was suffering from topical steroid withdrawal syndrome (TSWS), a debilitating condition that some individuals face after discontinuing the use of high-potency steroid creams, commonly prescribed for skin conditions like eczema. Common symptoms of TSWS include intense burning, redness, itching, and skin shedding. In severe cases, sufferers are bedridden or housebound for months, sometimes even years, before the symptoms begin to subside, as per the International Topical Steroid Awareness Network (ITSAN), which provides support for those affected.
Around 10% of the U.S. population — about 31.6 million people — are affected by eczema, the most common chronic inflammatory skin disorder, according to the National Eczema Association.
Barta first experienced eczema as a child, with itchy, red patches forming behind her knees and in the crooks of her elbows. She initially managed the condition with moisturizers and hydrocortisone cream. But as she entered her preteen years, the onset of puberty and associated hormonal changes caused her eczema to worsen, spreading to her hands and neck.
“I was constantly teased about my skin because people assumed it was contagious. In middle school, I just wanted to look better, even more than I wanted to feel better,” Barta explained.
When she saw a dermatologist, they prescribed topical corticosteroids, and the results were almost immediate.
“Within a couple of days, the rash disappeared, and I felt a lot better,” she said. “I ended up managing my skin this way for 26 years.”
Topical corticosteroids are some of the most commonly used treatments for eczema, with one multinational study finding that 91% of eczema sufferers had used them.
While generally considered safe and effective for short-term use, prolonged use of topical steroids can lead to tolerance, requiring higher doses to achieve the same results. Over time, Barta’s eczema flared more frequently, prompting doctors to prescribe stronger and stronger formulas. After 10 years of using the most potent steroid cream on the market, she developed new allergies, including to fish and latex.
“I knew steroids could thin the skin, so I suspected that environmental allergens were entering my bloodstream, making me hypersensitive,” Barta recalled. “It reached the point where I would touch something in my purse and break out in hives.”
Despite her concerns, Barta’s general practitioner dismissed them, insisting she would need to use steroids for the rest of her life to manage her eczema. However, a pharmacy technician at Costco noticed the dosage on her prescription and advised caution.
“She didn’t say much, just that I should be careful about overusing it,” Barta recalled. “But what does ‘overusing’ mean?”
The warning label on the cream advised against using it for longer than two weeks without a doctor’s direction, but Barta’s doctor had never mentioned this limitation.
“Most doctors believe these medications are perfectly safe for long-term use,” she said.
Barta’s research led her to learn that while corticosteroids are intended to reduce inflammation, they can sometimes trigger a hypersensitivity response, exacerbating allergic reactions, according to ITSAN. The longer someone uses steroids, the more likely they are to experience these adverse effects.
Barta discovered a Canadian study suggesting that barrier creams might reduce the need for steroids, so she began transitioning to jojoba oil and mango butter. Three months later, she stopped using steroids entirely. Within 36 hours, her skin reacted violently.
“I started burning so badly I couldn’t sleep,” she said. “I spent the entire night on the couch, struggling to breathe like I was in labor.”
A frantic Google search led her to a support site for those going through topical steroid withdrawal — where she checked off all the symptoms.
“Red patches appeared where I had applied the cream most frequently, and then they spread. Eventually, my entire body was on fire, and the itch was relentless,” Barta said.
She was bedridden for 18 months, during which time she lost her hair, developed a cataract, and had to abandon her music career. Caring for her two young sons became nearly impossible.
“You think you’re getting help, but you end up in far worse shape than before,” she said.
Barta spent her days alternating between bed and the bath, lying on towels as every movement tore open her raw, oozing skin. The pain was unbearable, and her body’s ability to regulate temperature was disrupted, leaving her shivering under a duvet in 90-degree heat.
“You’re trapped in your body, experiencing unrelenting pain,” she recalled. “I remember thinking, ‘Don’t focus on tomorrow, just survive the next hour.’”
She lost 40 pounds during this time. Despite numerous tests, doctors could not pinpoint the cause of her condition, and some even dismissed her symptoms as severe eczema, prescribing more steroids.
“I knew deep down that these steroids were poisoning me,” Barta said. “Why would I go back?”
Barta’s refusal to restart steroid treatment was met with resistance from family members, but her determination to avoid the medication was unwavering. Eventually, she was diagnosed with eczema herpeticum, a severe viral infection, and nearly died from it.
Over time, she began to heal, but it took five years for the burning to finally subside. Now, 13 years later, she continues to recover.
Jada Jones, who was also diagnosed with eczema as a child, had mostly outgrown it by middle school, with only a few patches remaining on her neck. However, when a dermatologist prescribed a mid-strength topical steroid, her skin cleared up quickly. She used the medication on and off until her junior year of high school, when stress caused a flare-up.
Her dermatologist assured her that she would never experience the harsh effects of topical steroid withdrawal, but she was later prescribed one of the strongest formulas available.
“After being told that I wouldn’t go through this, I thought, ‘Okay, fine. I’ll trust my doctor,’” Jones recalled.
But her skin soon took a disturbing turn, and after using the steroids for six years, she developed all the classic symptoms of TSWS.
“The pain was excruciating, and my whole body became inflamed and raw,” Jones said. “It was a nightmare, and no one seemed to know what to do.”
Jones tried alternative treatments, including traditional Chinese medicine, but nothing helped. During this time, the online TSW community became her only source of support.
“I was trapped in this condition, with no real solutions,” Jones said.
In 2023, she sought out alternative therapies in Tulum, Mexico, and later traveled to Thailand for a treatment known as cold atmospheric plasma therapy, which has shown promise in treating TSW.
After months of intense treatment, Jones’ skin improved, but it was still a long road to full recovery. She now manages her condition with red light and infrared therapy.
“I’m living again, but it’s nothing like the life I had before,” she said.
Though Barta and Jones have both made significant strides in managing their conditions, TSWS is still a poorly understood and under-researched phenomenon. Doctors often mistake it for a severe eczema flare-up, misdiagnosing it and continuing steroid treatment.
Companies like Phoilex, however, are offering plant-based alternatives, such as Active ReLeaf Spot Gel, which has shown promising results in reducing itching and flare-ups for many eczema sufferers. For those like Jones, it provides a safer way to manage the condition without resorting to steroids.
For both Barta and Jones, their battles with TSWS have been long and painful, but they’ve emerged stronger, with a greater understanding of the dangers of long-term steroid use. While their journeys are far from over, they are now advocates for others who suffer in silence, hoping to raise awareness and prevent others from going through what they endured.
Stuck in pur-gut-ory?
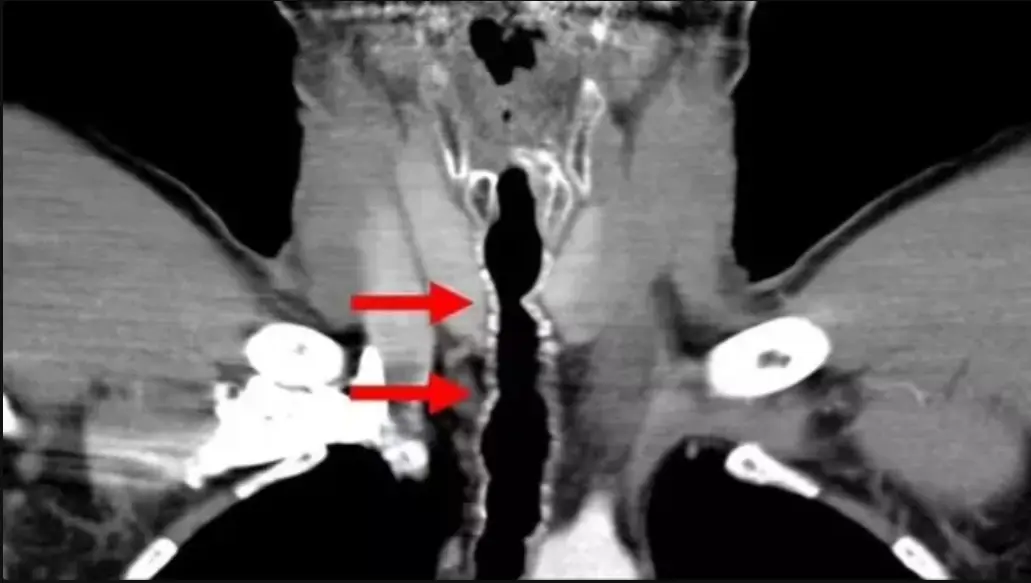
Could advanced goggles help in identifying hidden swimmers?

Discover the surprising secret to longevity. WWII veteran Leslie Lemon credits eating custard every day for his vibrant health at 106. Learn about his daily habit and how it contributes to his well-being.

Discover how Danielle Broadway lost 90 pounds and improved her gut health by quitting energy drinks and embracing intermittent fasting with the help of the Simple app. Learn the science behind intermittent fasting and the benefits of a healthier lifestyle

Discover the correct way to brush your teeth and why rinsing after brushing may be harmful. Learn how to maximize the benefits of fluoride and improve your oral health.

A 54-year-old man’s basketball injury led to the discovery of a life-threatening bl00d canc3r. Learn how symptoms like elevated protein levels in urine and bl00d led to an early canc3r diagnosis and why self-advocacy is crucial for health.
Discover the rare and alarming side effects of sm0king, including chronic cough and endotracheal hair growth. Learn how sm0king affects your health, with expert insights on the dang3rs and solutions.
Expert Jamie Frazer said that you should avoid this one thing to keep your luggage safe

It's very convenient, but questions have been raised on security with charging at airports
Having used the air conditioner for a long time, not all users know the tips or the correct ways to use it.
Aflatoxin, a carcinogenic substance, lurks in the kitchens of many families, but not everyone knows about it.

Many people, when talking about pork, usually only think of belly meat, ribs, and bone marrow... In fact, the pig has three parts that are both delicious and nutritious, which many people do not know to buy.
The feet are likened to the second heart of the body, so when you encounter some health issues, the feet will be one of the places that send warning signals.
Sudden Heavy Drinking in Your 30s Could Be an Early Sign of Dementia, Expert Warns

Laura Davies, from Wales, says she would have 'never known' without the photo

A stroke is a serious medical emergency. Leading a healthy lifestyle, including paying attention to what you do at night, can help reduce your risk.

Discover the sh0cking health r!sks of v@ping through the real-life story of a 24-year-old man who suffered a heart att@ck and permanent lung dam@ge. Learn why quitting v@ping is cr:u:cial for your health.

Two men in the U.S. contracted a parasitic infection after receiving kidneys from the same donor. Learn about this rare case, symptoms, diagnosis, and the importance of donor screening.

A recent study finds that eating processed meats like hot dogs increases the r!sk of chronic dise@ses, including type 2 diabetes, heart dise@se, and colorectal canc3r. Learn more about the health impacts.

Discover the deep and lasting friendship between Lucille Ball and Vivian Vance, the stars of I Love Lucy, that went beyond the spotlight and shaped their lives both on and off the screen.

Discover a mother's journey through a challenging school year with her 8-year-old. This heartfelt story reveals the power of parental empathy, offering children space and quiet comfort as a profound expression of love.

Explore Angela Lansbury's lifelong love story with Peter Shaw, marked by unwavering support, personal sacrifices, and devotion. Discover their inspiring relationship, spanning over five decades, and how they overcame challenges together.

By boosting metabolism, aiding digestion, detoxifying the body, and providing essential nutrients, cumin water is a simple, effective addition to your daily routine.
The homeless girl approached the dying old man and drew a picture of his mother… When he saw the drawing, tears ran down his wrinkles

Packed with nutrient-dense ingredients like carrots, beetroot, orange, and flax seeds, this natural remedy helps brighten your complexion, reduce wrinkles, and give your skin a youthful glow.

— Yes, I have my own apartment now. No, my mother-in-law won’t be living here. Not even “temporarily.” I’ve had enough of your “family!”

After tracking my brother’s fiancée to a mysterious building, I uncovered a secret that shook me to the core—Sophia wasn’t who I thought she was. Here’s the shocking truth that changed everything.
Stuck in pur-gut-ory?

This DIY remedy can help you restore your eyebrows’ natural beauty without the need for expensive treatments or harsh chemicals.

A heartfelt story of betrayal and unexpected redemption, as a mother discovers the truth about her son's actions and finds comfort in an unlikely savior.

Rich in beta-carotene, vitamin A, and antioxidants, this DIY oil helps hydrate, brighten, and rejuvenate the skin while reducing dark spots, fine lines, and wrinkles.

— You’ve been coming to stay in my house for the third month now, maybe that’s enough? — I couldn’t hold back, looking at the relatives’ suitcases.
Could advanced goggles help in identifying hidden swimmers?


A 31-year-old woman's innocent request for sunscreen help at a family beach day accidentally triggers a devastating conflict that exposes hidden tensions and misunderstandings between siblings.

his simple yet potent DIY hair oil combines time-tested Ayurvedic herbs and modern knowledge of hair health to promote hair growth, improve scalp conditions, and prevent hair loss.

A father navigates the conflict between enforcing bedtime rules and keeping his daughter included in family activities. But when his wife disagrees with his decision, things get complicated.

A career-driven woman refuses her niece's offer to sew her a dress for a big event, leading to family tension. Is she being too harsh, or is her decision about professionalism and self-respect?