
What Causes Blue Veins? Understanding the Reasons and When to Seek Help
Have you ever looked at your skin and wondered, “Why are my veins so blue?” The appearance of blue veins can be caused by several factors, ranging from harmless genetic traits to more concerning health conditions. While it is typically normal to have visible veins, understanding the reasons behind their color and appearance can help you know when to seek professional advice.
This article explores the causes of blue veins, the factors that can make veins more prominent, and the health conditions that may cause visible veins to signal something more serious.

Why Are My Veins Blue? Understanding the Causes
There are various reasons why your veins may appear blue, with some of the most common ones being:
-
Light Absorption and How Your Eyes Process It
The color of your veins can be influenced by how light interacts with your skin. Your veins appear blue because your skin absorbs other colors in the light spectrum, and the blue wavelength is reflected back to your eyes. -
Skin Color and Complexion
People with lighter skin tones are more likely to notice prominent veins because the skin is thinner, making veins more visible. Those with darker skin tones may not see veins as clearly, but this doesn't mean they are absent. -
Genetics
In some cases, genetics play a role in how visible veins are. If your family members have prominent veins, you might be more likely to have them as well. -
Hormonal Changes
Hormones can impact how veins appear. Pregnancy, menopause, and puberty can cause veins to become more noticeable, especially in areas like the legs and feet. -
Age
As you age, your skin becomes thinner and loses elasticity, making veins more visible. Additionally, the veins may become more dilated over time, leading to a more pronounced appearance. -
Weight or Body Mass Index (BMI)
A higher body fat percentage can make veins less visible, as the fat layer may hide them. Conversely, people with lower body fat might notice more prominent veins, particularly in the arms and legs. -
Blood Properties
Blood circulation can impact the visibility of veins. Poor circulation or blood pooling in certain areas may lead to more noticeable veins.
When Are Blue Veins a Sign of a Medical Condition?
While visible veins can be a normal part of your body’s makeup, there are situations where the appearance of blue veins could indicate an underlying medical issue. Some conditions that may be associated with noticeable or painful veins include:
-
Varicose Veins
Varicose veins are enlarged, twisted veins, often found in the legs and feet. They are caused by weak or damaged vein walls and valves, leading to blood pooling in the veins. These veins can become blue and bulge out. -
Deep Vein Thrombosis (DVT)
DVT occurs when a blood clot forms in a deep vein, typically in the legs. It can cause the veins to appear blue or dark in color. This condition is serious and can lead to life-threatening complications if not treated. -
Superficial Venous Thrombosis
This condition involves clotting and inflammation just beneath the skin, which may cause veins to appear rope-like and dark in color. -
Venous Ulcers
Venous ulcers are open sores that develop due to poor circulation in the legs. They are often associated with visible blue veins and can be painful and slow to heal. -
Chronic Venous Insufficiency
This occurs when the veins can’t pump blood back to the heart effectively, leading to blood pooling in the legs. It can cause the veins to become enlarged and turn blue, often accompanied by swelling and skin changes. -
Lymphedema
Lymphedema involves swelling, typically in the arms or legs, caused by poor lymphatic fluid drainage. It can also cause veins to appear more prominent and may be associated with other visible signs like skin discoloration.
Lifestyle Habits That Can Contribute to Blue Veins
Certain lifestyle factors can make veins more prominent, particularly in the legs and feet. These include:
-
Prolonged Sitting or Standing
Long hours of inactivity, especially in professions that require prolonged sitting or standing, can slow blood flow and cause blood to pool in certain areas of the body, making veins more noticeable. -
Strenuous Activity
Intense physical activity increases blood pressure and causes veins to expand. While this is often temporary, it can make veins more visible during and after exercise. -
Alcohol Consumption
Excessive alcohol intake can increase heart rate and blood pressure, which can make veins more noticeable, particularly in the legs. -
Smoking
Nicotine and other chemicals in cigarettes damage the lining of blood vessels, making it harder for the veins to function properly. This can cause them to constrict and become more visible. -
Obesity
Being overweight can put extra pressure on your veins, causing them to dilate and appear more pronounced, especially in the lower body.
When to Seek Professional Help
If your blue veins are accompanied by any of the following symptoms, it’s important to consult a healthcare provider for evaluation:
-
Bulging veins that are painful or uncomfortable
-
Heaviness or cramping in the legs
-
Itching around the affected veins
-
Skin discoloration or changes in skin texture
-
Swelling in the feet, ankles, or legs
A medical professional can assess whether your veins are simply a cosmetic concern or if they indicate a more serious condition that requires treatment.
Conclusion
Blue or green veins are usually harmless, and many people have them as part of their normal anatomy. However, visible veins that are accompanied by pain, discomfort, or other symptoms may point to a more serious health issue, such as varicose veins, deep vein thrombosis, or chronic venous insufficiency.
If you notice changes in your veins or experience discomfort, it’s best to consult a healthcare provider for a proper diagnosis and treatment plan. Early intervention can prevent complications and ensure better long-term health.
Credit: This article is based on expert insights and information from Healthline, Cleveland Clinic, and Mayo Clinic. For more details on vein health and related conditions, visit reputable sources like Healthline and consult a healthcare professional for personalized advice.
News in the same category


Restore Your Grout Lines with This Easy and Budget-Friendly DIY Cleaning Hack

12-Year-Old's Lifelong Dialysis: 5 Favorite Foods Secretly Damaging Your Kidneys

Eating While Screen-Obsessed? Here Are 4 Hidden Health Risks You’re Ignoring

How to Choose the Sweetest Pineapple: Long Leaves or Short?

8 Simple Yet Highly Effective Tips to Stop Snoring

Is It Necessary to Unplug Your Washing Machine After Use

The Hidden Costs of Frost Accumulation in Your Refrigerator: Understanding the Energy Drai

🍎 Why Do Imported Apples Stay Fresh for a Month Without Spoiling?

Top 3 Seat Positions with the Highest Survival Rates in Aviation Emergencie
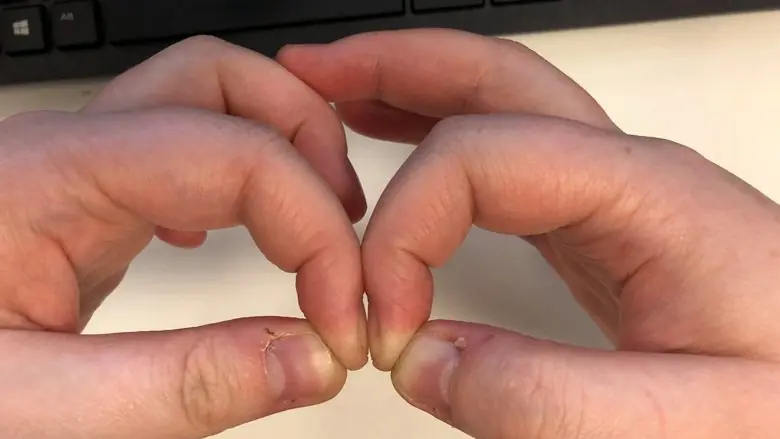
Simple Finger Test Could Reveal Early Signs of Lung C@ncer and Other Health Issues
A simple finger test, known as the Schamroth window test, can help detect signs of lung c@ncer and other health conditions, including heart problems. Learn how to perform this easy test at home.

Start Your Day Right: 5 Foods That Safeguard Your Kidneys and Reduce Uric Acid

The Ultimate Health Blend: Honey, Cinnamon, Turmeric, Apple Cider Vinegar, and Chia Seeds for Better Health
Discover the powerful benefits of honey, cinnamon, turmeric, apple cider vinegar, and chia seeds. Learn how this natural blend can improve digestion, stabilize blood sugar, and enhance bone and heart health.
Revolutionary C@ncer Treatment: Doctors Target Tumors Without Chemotherapy

Why Your Underwear Gets Bleach-Like Stains: Gynecologist Explains the Causes and What It Means for Your Health
Discover why your underwear may have bleach-like stains and why it's completely normal. A gynecologist explains the role of vag!nal discharge and how it can affect your underwear fabric. Learn when to be concerned and how to maintain vag!nal health.

12 Effective Ways to Remove a Wart on Your Finger
Discover effective methods for removing warts on your fingers, from at-home remedies like salicylic acid and duct tape to professional treatments. Learn how to identify, treat, and prevent warts with expert advice.

5 Household Items That Harbor Formaldehyde: Hidden Cancer Risks Lurking in Your Home
Air Conditioner Efficiency: Continuous Use vs. Frequent Switching

What Homebuyers Need to Know: 5 Locations to Avoid When Buying Property
Don't plant these 5 trees indoors: The more they thrive the more they're believe to drain human energy, attracting constant bad luck
News Post

Beyond the BuII!e$: How One Girl Stitched Her Way Back to Confidence with Crochet
After facing buIIy!ng for her unique style, a 6th-grade girl found her voice and confidence again through crochet. Discover this inspiring story of artistic triumph, self-expression, and how handmade passion can build an empire, one stitch at a time.

Long vs. Round Eggplants: Which One Should You Choose?

The Heartbre@king Selfie: A Dream Shattered in the Blink of an Eye
On June 12, a family’s dream of a new life in London ended tragically in a plane crash. Discover the emotional story of Pratik Joshi’s family, their dreams, and the reminder that life is fragile.

Restore Your Grout Lines with This Easy and Budget-Friendly DIY Cleaning Hack

12-Year-Old's Lifelong Dialysis: 5 Favorite Foods Secretly Damaging Your Kidneys

5 DIY Skin Toners for Radiant, Smooth Skin: Natural Remedies for Every Skin Type
By incorporating these simple DIY toners into your daily skincare regimen, you can achieve smoother, clearer, and more radiant skin without the need for expensive products.

Eating While Screen-Obsessed? Here Are 4 Hidden Health Risks You’re Ignoring

Should You Stay or Let Go? How I Realized I Wasn't His First Choice
A heartfelt and emotional journey of love, heartbreak, and self-discovery. When your partner is still hung up on their ex, is it worth fighting for the relationship? Discover the painful truth behind choosing yourself over unrequited love.

Vaseline and Coffee: The Ultimate DIY Skincare Duo to Achieve Wrinkle-Free Skin Naturally
By incorporating these ingredients into your skincare routine through DIY masks and scrubs, you can rejuvenate your skin, reduce the appearance of wrinkles, and achieve a youthful, radiant complexion.

The Flowers that Kept Us Apart: A Love Story Decades in the Making
A woman embarks on a journey to find out the truth behind mysterious flowers sent to her every year, only to uncover a love story that had been hidden for 20 years.

I Found My Husband's Secret Conversations With Another Woman – And What He Told Me Br0ke My Heart
A wife discovers her husband's secret texts with a woman he met at a strip club. What seemed like innocent conversations quickly turns into an affair, and now she has to decide if she can ever trust him again.

Weight Loss Drink: Consume These 2 Herbal Drinks To Detox and Lose Weight Naturally
These two natural detox drinks-Spiced Lemon-Honey Drink and Cumin Water-are simple yet powerful remedies for boosting metabolism, improving digestion, and reducing belly fat.

How to Choose the Sweetest Pineapple: Long Leaves or Short?

Abandoned Child, Heartbre@king Note, and the Sh0cking Truth Behind a Family's Dark Secret
When a woman discovers an abandoned child with a mysterious note, she’s thrust into a tangled web of secrets, betrayal, and an inheritance that changes everything. Dive into this captivating story of hidden truths and the love that saves a life.

8 Simple Yet Highly Effective Tips to Stop Snoring

Is It Necessary to Unplug Your Washing Machine After Use

4 Natural Potato Remedies to Fade Dark Spots and Achieve Even Skin Tone
Potatoes are a natural and effective solution for treating dark spots, pigmentation, and uneven skin tone.

The Hidden Costs of Frost Accumulation in Your Refrigerator: Understanding the Energy Drai

Homemade Vitamin C Serum: DIY Recipe for Clear, Glowing, and Ageless Skin
A homemade Vitamin C serum is a natural, affordable, and effective way to achieve radiant, youthful skin.
