Understanding Nail Pitting in Psoriasis
What Is Nail Pitting?
Nail pitting refers to the presence of small depressions or dents on the surface of the nails. These pits can vary in size and depth and are often associated with psoriasis, an autoimmune condition that accelerates skin cell turnover. While nail pitting can occur independently, it frequently manifests alongside other psoriasis symptoms, such as skin plaques and joint inflammation.
Prevalence and Risk Factors
Approximately 50% of individuals with psoriasis experience nail changes, with nail pitting being one of the most common manifestations. The condition is more prevalent in those with psoriatic arthritis, affecting up to 80% of patients. Genetic predisposition, immune system dysfunction, and environmental triggers like trauma or infections can increase the risk of developing nail pitting.
Symptoms Associated with Nail Pitting
Beyond the characteristic dents, nail pitting may be accompanied by:
-
Discoloration: Yellowish or brownish spots beneath the nail plate, known as "oil drop" or "salmon patch" signs.
-
Thickening: Nails may become thickened or brittle, leading to crumbling.
-
Onycholysis: Separation of the nail from the nail bed, potentially causing pain and discomfort.
-
Beau’s Lines: Horizontal grooves that can appear across the nails.
These symptoms can vary in severity and may affect one or more nails.
Diagnosing Nail Pitting in Psoriasis
Diagnosis primarily involves a clinical examination by a dermatologist. The presence of nail pitting, along with other psoriasis symptoms, can lead to a diagnosis of nail psoriasis. In cases where the diagnosis is uncertain, additional tests such as potassium hydroxide (KOH) preparation or fungal cultures may be conducted to rule out fungal infections. A biopsy of the nail matrix might be considered in atypical cases.
Treatment Options for Nail Pitting
Managing nail pitting involves addressing the underlying psoriasis and alleviating nail-specific symptoms. Treatment strategies include:
1. Topical Treatments
-
Corticosteroids: Topical steroids can reduce inflammation and are commonly applied to the affected nails.
-
Vitamin D Analogues: Calcipotriol and calcitriol help normalize skin cell production.
-
Retinoids: Tazarotene, a vitamin A derivative, can improve nail appearance.
2. Intralesional Steroid Injections
For localized and severe cases, corticosteroid injections directly into the nail matrix can provide relief. This method targets inflammation at the source but may be painful.
3. Systemic Therapies
In cases resistant to topical treatments, systemic medications may be prescribed:
-
Methotrexate: Suppresses immune system activity.
-
Cyclosporine: Inhibits T-cell activation.
-
Apremilast (Otezla): Oral medication that reduces inflammation.
-
Biologics: Drugs like adalimumab (Humira) and secukinumab (Cosentyx) target specific immune pathways.
4. Phototherapy
Ultraviolet light therapy, particularly PUVA (psoralen plus UVA), can be effective in treating nail psoriasis by slowing skin cell turnover.
5. Laser Therapy
Pulsed dye laser (PDL) therapy targets blood vessels under the nail, reducing inflammation and promoting healing.
Home Care and Lifestyle Recommendations
While medical treatments are essential, home care practices can support nail health:
-
Moisturization: Regularly apply emollients to keep nails hydrated.
-
Nail Protection: Wear gloves during activities that may cause trauma to the nails.
-
Avoid Trauma: Prevent nail injury, as it can exacerbate psoriasis symptoms.
-
Dietary Considerations: Incorporate anti-inflammatory foods and consider supplements like omega-3 fatty acids.
-
Avoid Smoking and Excessive Alcohol: These can trigger or worsen psoriasis flare-ups.
Prognosis and Outlook
Nail pitting associated with psoriasis is a chronic condition that may fluctuate in severity. While treatments can manage symptoms, complete resolution is rare. Early intervention and consistent management are crucial in preventing complications and maintaining nail function.
When to Consult a Dermatologist
Seek professional advice if you experience:
-
New or worsening nail changes.
-
Pain or discomfort in the nails.
-
Signs of infection, such as redness or pus.
-
Difficulty performing daily tasks due to nail involvement.
A dermatologist can provide a tailored treatment plan to address your specific needs.
News in the same category

36-Year-Old Teacher Passed Away From Diabetes Doctors Say Was Triggered By Everyday Foods
Diabetes is a dangerous condition with numerous complications, and diet is a key factor.

Experts issue urgent warning about terrifying hidden symptom from taking Mounjaro and Ozempic
Experts have issued an urgent warning about a symptom that can come to light from taking drugs such as Mounjaro and Ozempic.

The Benefits of Epsom Salt Foot Soak: A Natural Remedy for Foot Pain and Health
Discover the health benefits of Epsom salt foot soaks, including pain relief, exfoliation, fungal infection treatment, and more. Learn how to safely use Epsom salt for foot health.

What Causes Blue Veins? Understanding the Reasons and When to Seek Help
Blue or green veins are common, but when should you worry? Learn the possible causes of visible veins, from genetics to lifestyle factors, and when it may indicate a medical condition.

7 Early Warning Signs of Diabetes You Shouldn’t Ignore: Act Now for Better Health
Learn about 7 early warning signs of diabetes that could be easily overlooked. Early detection can help manage diabetes, prevent complications, and improve quality of life. Read on for expert insights.

Genetic Link Between Endometriosis and Autoimmune Diseases Revealed in New Study
A new study has identified a shared genetic link between endometriosis and autoimmune conditions. Women with endometriosis are at a higher risk for diseases like rheumatoid arthritis, multiple sclerosis, and psoriasis.

People Warned to See a Doctor After Sharing Photo of Concerning Dark Line on Finger
A Reddit user received warnings to see a doctor immediately after posting an image of a dark line on their finger. Learn about melanonychia and why nail discoloration can be a serious health concern.
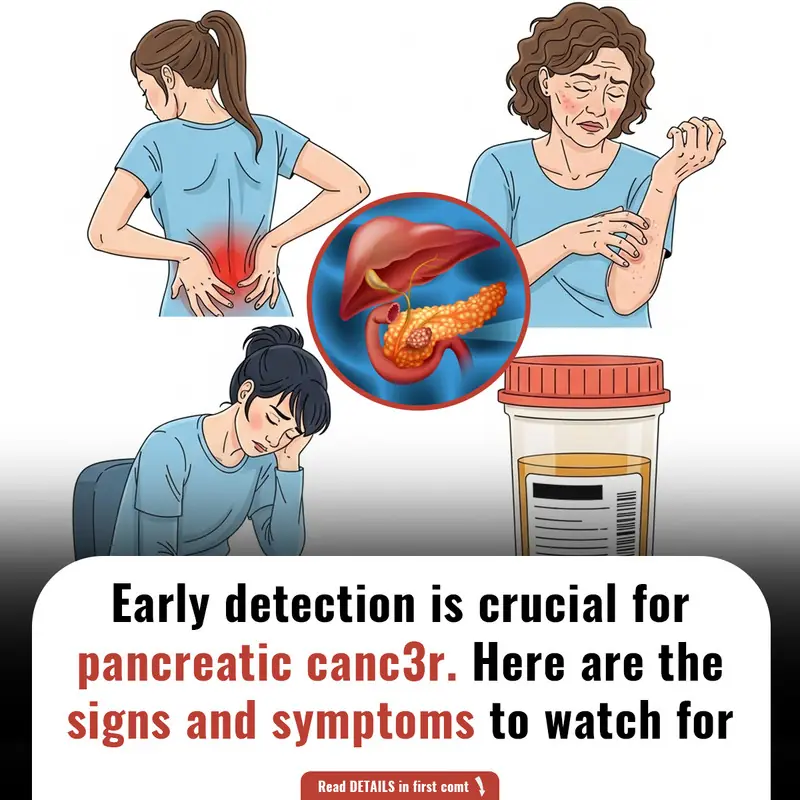
Breakthrough in Parkinson’s Treatment: Japanese Scientists Successfully Implant Lab-Grown Brain Cells
Japanese researchers have made a groundbreaking discovery in Parkinson’s treatment using lab-grown brain cells. Early results from the clinical trial show promising improvements in movement and dopamine production.

4 Simple Steps to Cool Your Home Faster and Save on Electricity Before Turning on the Air Conditioner
3-Blade vs. 5-Blade Fans: Which Cools Better? The Truth Behind Common Misconceptions
The Alarming Rise of Bowel C@ncer in Young Adults: Is Your Diet to Blame

United Airlines Passenger Punches Gate Agent, Kn0cking Them Out

Should You Close or Leave the Toilet Lid Open After Use? 90% of People Get It Wrong — Here's Why Your Bathroom Always Smells
4 Everyday Foods That Fuel C@ncer Cells

Fatty Liver Disease: A Silent Pathway to Liver C@ncer

The Hidden Purpose of the Pocket in Women's Underwear: More Than Just a Design Feature
In actuality, the "pocket" in women's underwear is actually a gusset, which serves a number very valid purposes.
This quick 'cup of tea' test could be a simple way to spot early signs of dementia in a loved one
A doctor has revealed a simple thumb test that can uncover a "ticking time b0mb" heart condition
Avocados are incredibly healthy, if using them incorrectly in these 3 common ways could actually have adverse effects
News Post

The Woman Who Walked Away: A Journey of Self-Discovery and Empowerment
A powerful tale of self-realization as Alina breaks free from a toxic relationship, finding strength and confidence after a painful breakup. Discover how she chooses her own path towards happiness and independence.
Silent Signals: Recognizing the Subtle Symptoms of Pancreatic C@ncer

The Earring in the Passenger Seat: A Suspicious Find Leads to a Truthful Confrontation
A woman finds a sh0cking truth after discovering a mysterious child’s drawing in her fiancé’s car. Suspicion, betrayal, and secrets unravel as she confronts him, ultimately deciding the fate of their relationship.

Am I Wrong for Not Laughing at My Fiancé's "Jokes" About Calling Off Our Wedding?
A bride-to-be is questioning her relationship after her fiancé repeatedly jokes about calling off their wedding. What happens when humor crosses the line into hurtful behavior?

36-Year-Old Teacher Passed Away From Diabetes Doctors Say Was Triggered By Everyday Foods
Diabetes is a dangerous condition with numerous complications, and diet is a key factor.

Experts issue urgent warning about terrifying hidden symptom from taking Mounjaro and Ozempic
Experts have issued an urgent warning about a symptom that can come to light from taking drugs such as Mounjaro and Ozempic.

The Benefits of Epsom Salt Foot Soak: A Natural Remedy for Foot Pain and Health
Discover the health benefits of Epsom salt foot soaks, including pain relief, exfoliation, fungal infection treatment, and more. Learn how to safely use Epsom salt for foot health.

What Causes Blue Veins? Understanding the Reasons and When to Seek Help
Blue or green veins are common, but when should you worry? Learn the possible causes of visible veins, from genetics to lifestyle factors, and when it may indicate a medical condition.

DIY Rice Cream for Radiant, Youthful Skin: The Japanese Secret to Erasing Wrinkles & Fine Line
With its powerful combination of rice, almond oil, and vitamin-rich ingredients, this rice cream provides nourishment, hydration, and antioxidant protection to your skin.

7 Early Warning Signs of Diabetes You Shouldn’t Ignore: Act Now for Better Health
Learn about 7 early warning signs of diabetes that could be easily overlooked. Early detection can help manage diabetes, prevent complications, and improve quality of life. Read on for expert insights.

5 Homemade Skin Toners for Smooth, Glowing Skin: Natural Remedies for Every Skin Type
By incorporating these toners into your daily routine, you can expect healthier, brighter, and more balanced skin without the use of harsh chemicals.

Genetic Link Between Endometriosis and Autoimmune Diseases Revealed in New Study
A new study has identified a shared genetic link between endometriosis and autoimmune conditions. Women with endometriosis are at a higher risk for diseases like rheumatoid arthritis, multiple sclerosis, and psoriasis.

Roasted Onion Peel and Garlic Peel Remedies for Grey Hair: Natural Solutions for Dark, Vibrant Hair
. Roasted onion peel and garlic peel offer effective, safe, and natural alternatives that can help you combat grey hair and restore youthful vitality.

People Warned to See a Doctor After Sharing Photo of Concerning Dark Line on Finger
A Reddit user received warnings to see a doctor immediately after posting an image of a dark line on their finger. Learn about melanonychia and why nail discoloration can be a serious health concern.
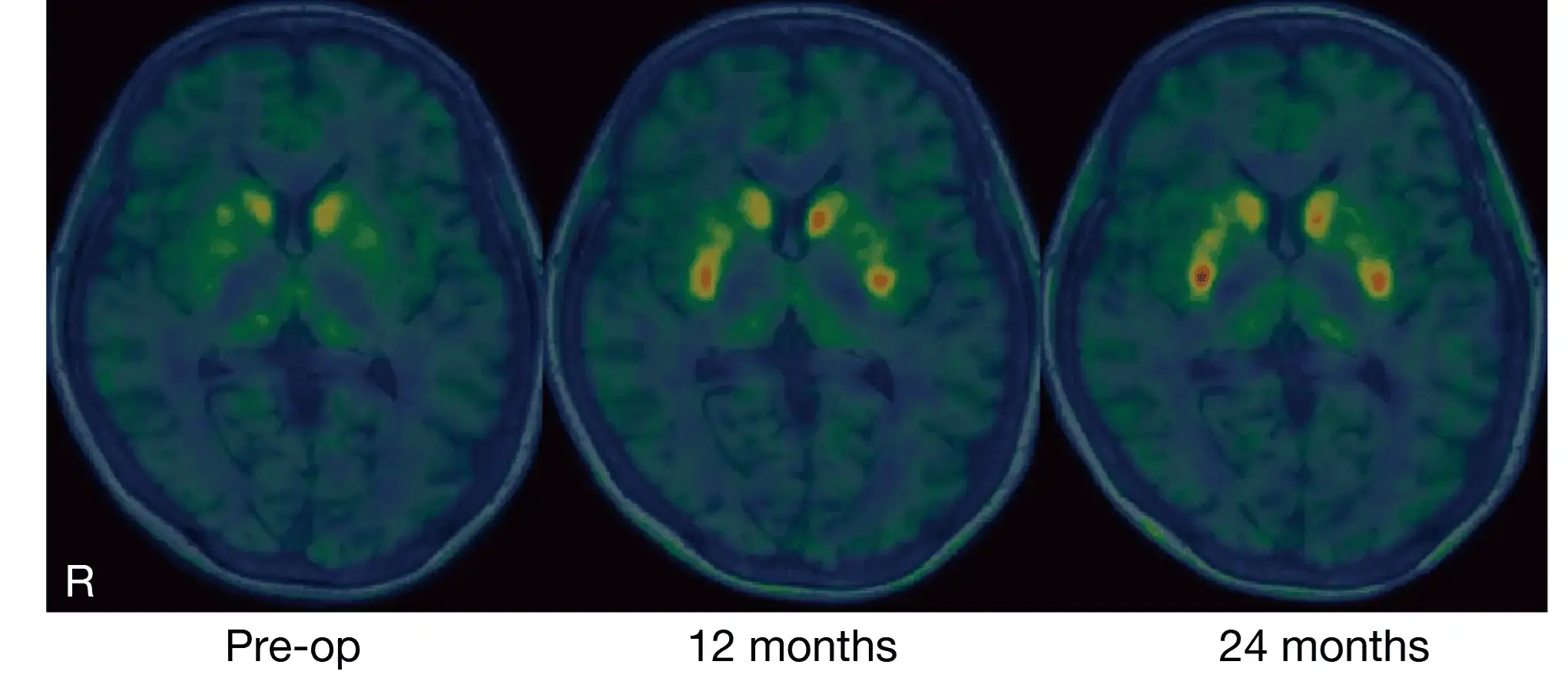
Breakthrough in Parkinson’s Treatment: Japanese Scientists Successfully Implant Lab-Grown Brain Cells
Japanese researchers have made a groundbreaking discovery in Parkinson’s treatment using lab-grown brain cells. Early results from the clinical trial show promising improvements in movement and dopamine production.

4 Simple Steps to Cool Your Home Faster and Save on Electricity Before Turning on the Air Conditioner

Effective Cumin Seed Detox Tonic for Belly Fat Reduction: Your Ultimate Guide to a Flatter Midsection
The cumin seed detox tonic is a natural, easy-to-make remedy that can help accelerate belly fat loss, improve digestion, and enhance overall health.
3-Blade vs. 5-Blade Fans: Which Cools Better? The Truth Behind Common Misconceptions
The Alarming Rise of Bowel C@ncer in Young Adults: Is Your Diet to Blame
