Unaware of his rare canc3r, man donates sp3rm to conc3ive at least 67 children across Europe - resulting in deva$tating consequences

A molecular biologist specializing in human genetics at Rouen University Hospital, Dr. Kasper led the research identifying the cancer-causing TP53 mutation in the donor sperm. She is a vocal advocate for stricter regulatory frameworks in fertility treatments and the responsible use of genetic data.
Professor of Bioethics and Health Law at De Montfort University, Leicester, Professor Hudson researches ethical, legal, and social issues in genetics and assisted reproduction. She emphasizes the complexities and risks of cross-border gamete donation.
News in the same category

Study finds certain blood types linked to higher stroke risk

After tens of thousands auditions, Harry Potter's next generation cast revealed

Cia documents reveal cold war secrets of alien bases hidden on earth

Woman who claims 12 years of contact with a ghost reveals h@unting prediction for the world's end

Teacher Awarded $70 Million After Losing Both Legs Due to Medical Malpractice in Landmark Georgia Case

Why swimming post-tattoo can be fat@l: Lessons from a 31-year-old man’s d3ath

Highly intelligent people often thrive with fewer friends — and the fascinating reason behind it

Woman battling stage four colon canc3r reveals major symptom that didn't involve her gut

Early warning signs and symptoms of clogged arteries that you might overlook

Psychic who 'predicted Covid' shares incredibly worrying predictions for 2025 warns of d!sturbing events in the latter half of 2025

Scientists may have discovered one of the causes of auti$m

Ancient Submerged City Discovered Beneath the Ocean Floor – A 140,000-Year-Old Window into Prehistoric Life

What your face might reveal about your future children: scientists explore the surprising link between male features and child gender
Unveiling the Truth: Why 2XL and XXL Are Not the Same—A Deep Dive into Plus-Size Fashion Sizing

10 cities underwater by 2050 you should visit before it’s too late
17 C@ncer Symptoms You Should Never Ignore: Early Warning Signs for Better Outcomes

Groundbreaking study sheds light on possible true appearance of Jesus, and it changes everything

Chef who prepares last meals at hospice for people at end of lives says they have have one common request
News Post
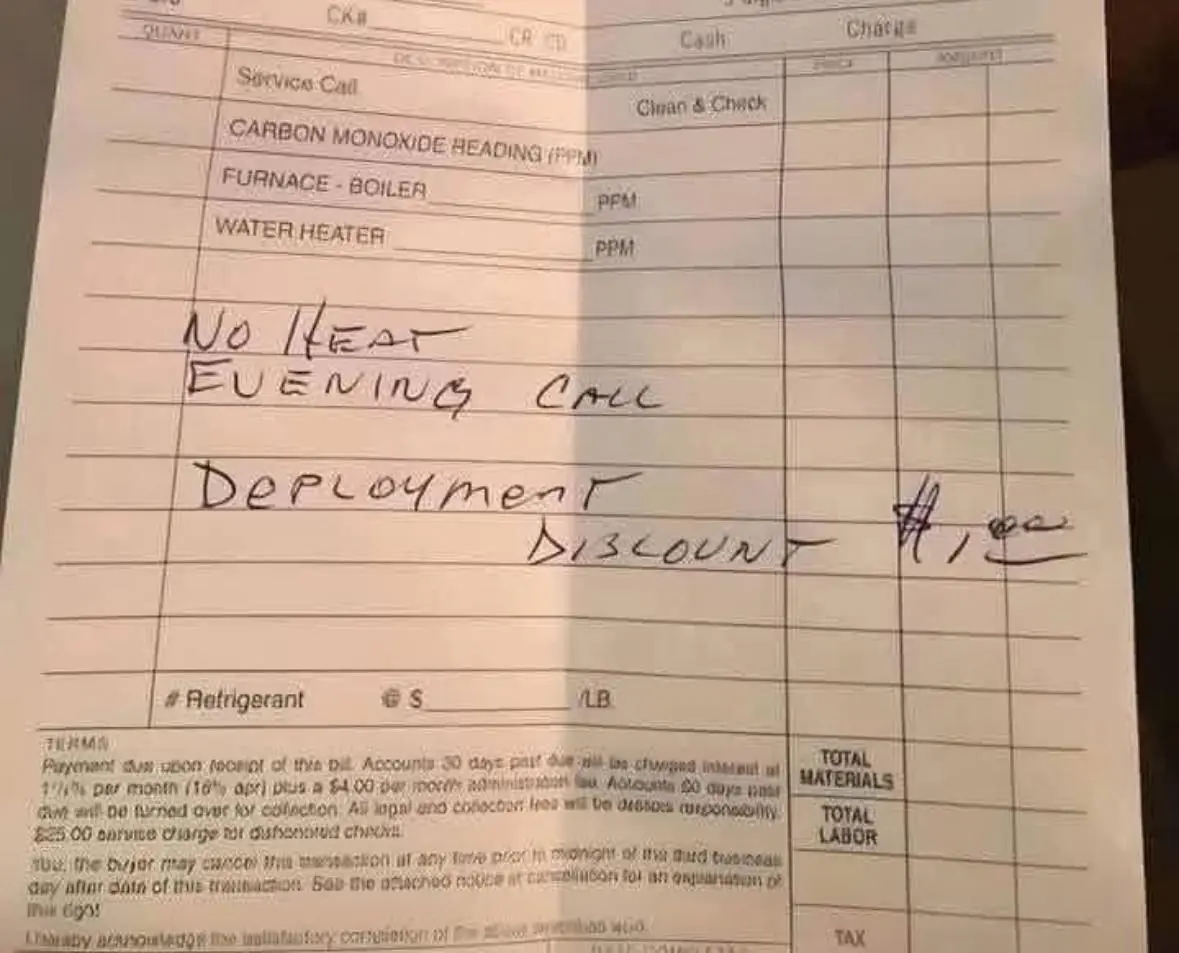
A Heartwarming Act of Kindness: How One HVAC Owner Saved a Family’s Winter—and Honored a Deployed Soldier
When a family’s furnace failed on a freezing night, a heating company owner went above and beyond—fixing the problem and charging just $1 in a touching tribute to military service. Discover the inspiring story of generosity and gratitude that warmed m

Officer Reese’s Compassionate Response: A Heartwarming Moment at Starbucks
Officer Reese calms an upset man at Starbucks with empathy, showing true kindness. Read this story! ❤️☕

At her mother’s wedding, the girl took the microphone to congratulate her but instead showed a sh0cking video.

The Hidden Key in His Work Boot: Uncovering a Secret Life and the Shattered Marriage That Followed
When I found a mysterious second key hidden in my husband’s work boot, it unraveled a web of l!es, a secret child, and a hidden life. This is the gripping story of betrayal, heartbre@k, and the pa!nful journey toward truth and unexpected reconciliation.

After Betrayal: How One Woman Found Strength and Reclaimed Her Life from a Br0ken Marriage
After 32 years of marriage shattered by betrayal, Lidia discovers her inner strength and dignity. This gripping story reveals her journey from heartbreak to empowerment, showing how she turned pain into a new beginning.

When a Wedding Gift Sparks a Family Fallout: The Sh0cking Truth Behind the Missing Wedding Video
At her niece’s lavish wedding, a grandmother’s heartfelt gift is cr:u:elly dismissed, igniting a dramatic family clash. Discover how love, legacy, and justice prevailed amid the mysterious disappearance of the wedding video and shattered illusions.

Unearthing Betrayal: How a Hidden Box Sparked My Journey from Heartbre@k to Healing and New Love
After discovering a hidden box revealing years of lies beneath my garage floorboards, I faced the crushing truth of betrayal. A year later, I found strength, reclaimed my life, and embraced new love.

4 household appliances that are energy hogs and how to tame them

5 Common Electric Kettle Mistakes That Could Lead to Serious Accidents

Why Dogs Are More Sensitive and Alert During Thunderstorms Than Humans: The Science Behind Their Unique Instincts

When a 911 Call Changed Everything: The Heartwarming Story That Proves Heroes Walk Among Us
Discover how a compassionate 911 operator went beyond duty to help a starving cancer survivor, sparking a community movement of kindness that will restore your faith in humanity.

Why Experts Recommend Putting Your Luggage in the Bathtub After Checking in: Turns Out It Has Many Unexpected Benefits

Experts reveal the effects on your body from eating one meal a day after a sh0cking simulation
Major medical breakthrough: Korean researchers discover “Undo” mechanism to transform tumor cells back to normal
If you often notice ringing in your ears, this might be a sign that you will suffer from ...

Drink water on an empty stomach right after waking up for 1 month and see how you transform physically and mentally

MY STEPMOTHER K!CKED ME OUT AFTER DAD'S DE@TH - THEN THE BLACK SUVs SHOWED UP
When Elish loses her father, she expects grief, not betrayal. K!cked out of her childhood home by the woman who never wanted her, she makes one desperate call. But what waits on the other end isn’t pity but power.

Collagen Drops from Flaxseed Gel: A Natural Botox Alternative for Youthful, Wrinkle-Free Skin
Flaxseed collagen drops offer a compelling, natural alternative to invasive anti-aging treatments like Botox.
5 types of food that can do wonder for your gut health and digestion
